Our priority outcome: To increase the number of people able to live independently.
Our approach is to support people to live in the community as independently as they are able. This means keeping down the time they are in hospital or places with full-time supervision to the minimum required, and only when they really need this much support

Context and key challenges
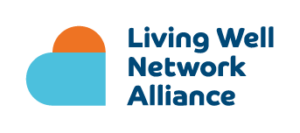
We used an average of 85 acute (hospital) beds in 2023/24 the lowest for five years (other than the pandemic year of 2020/21) and a big reduction from the 91 beds used in the previous year. However, this remains above the 81 beds that Lambeth has available which means that we had to use private beds costing over £2m, and likely to be outside Lambeth. We continue to see a high number of people from outside Lambeth, and a significant number from outside London and even outside the UK. Many patients are homeless or ineligible for welfare benefits, which means it takes longer to discharge them when they are well enough
What we offer
The whole Alliance system is working to help people with enduring mental health challenges to live independently as soon as they possibly can.
Community Liaison and Support Service (CLaSS)
Our Community Liaison and Support Service (CLaSS) works with our inpatient staff and peers (people with lived experience) who work with people in wards to build confidence and identify and resolve any issues that may prevent them from moving on once they are well enough. This includes housing and financial issues and tackling practical issues such as hoarding.
Culturally Appropriate Peer Support and Advocacy (CAPSA)
Our pioneering Culturally Appropriate Peer Support and Advocacy (CAPSA) service provides support (including on wards) for those from our Black communities to reduce the inequalities in access, experience and outcomes of these communities.
Living Well Centre: Short-Term and Focused Support Teams
Our Living Well Centre Short Term and Focused Support Teams regularly review those they support, to ensure they are receiving the right level of care.
PCAN (Primary Care Alliance Network)
PCAN (Primary Care Alliance Network) involves GPs, Mental Health Practitioners and other community based health specialists meeting with Alliance Living Well Centre staff, on a fortnightly basis, to support more people in their homes and communities. Our innovative Staying Well offer works alongside PCAN to provide practical support for more people to live independently.
Supported Accommodation
We buy a large number of ‘supported accommodation’ services. These range from a few hours a week supporting someone in their own home (for example to ensure medication is taken) to 24 hour supported specialist accommodation for those with greater needs. We have recently refreshed many of these contracts to improve the support provided and make it more relevant to the needs of those we support.
Home First
We piloted a ‘Home First’ service, to provide more intensive support to people straight back to their own homes rather than to go into supported accommodation or other less independent settings.
Our impact
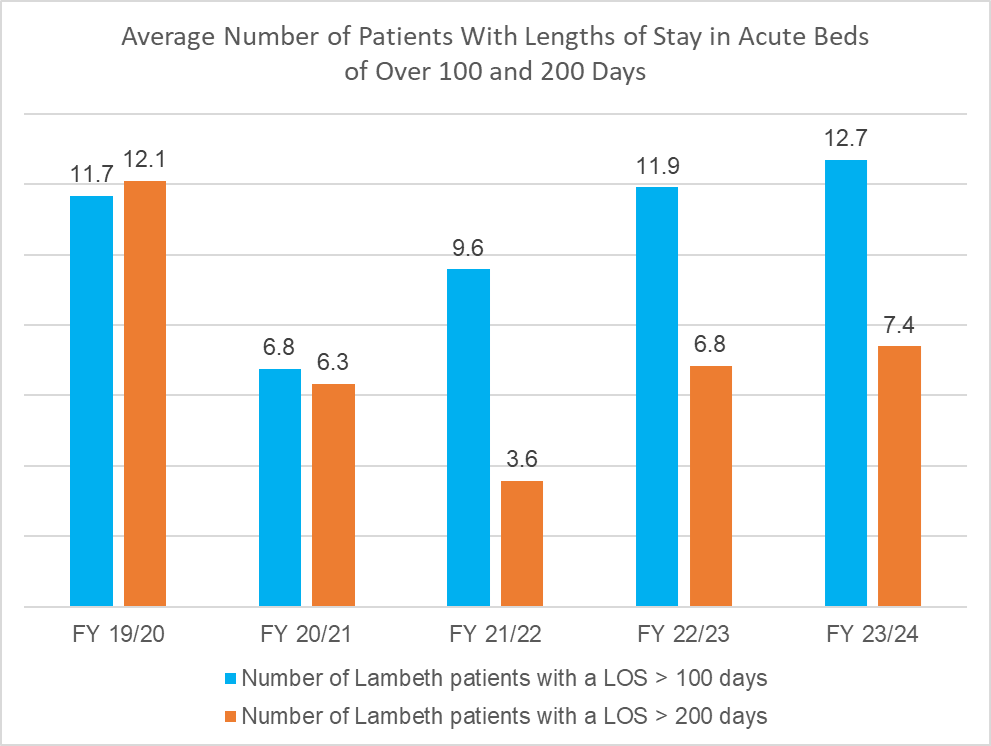
As the chart shows, 2023/24 continued to see increases in long lengths of stay in acute beds (more than 100 days and more than 200 days). As stated above, the high number of patients who are homeless and/or ineligible for welfare benefits means it takes longer to find them somewhere when they are well enough to be discharged.
Our Home Treatment Team, which works with people to keep them out of hospital, supported 843 people in 2023/24, up 8% on the previous year.
Our Focused Support Teams supported on average 714 people in 23/24, which is 10% fewer than the previous year and discharged 335 people, 47% of their average caseload.
Our Short Term Support Teams discharged 814 people in 2023/24 against an average caseload of 480.
Our Home First Team worked with 90 people in their first six months
Our next steps
We recognise we need to reduce the number of people experiencing long-term hospital stays. We’re continuing to improve the way we work so people can have greater independence sooner by:
- reviewing how we make referral and discharge decisions, finding and addressing anything that may be preventing someone from being discharged sooner.
- improving supported accommodation services,
- developing and expanding our Staying Well approach,
- introducing new roles such as community reablement workers, mental health practitioners in GP surgeries and transitions workers for children and young people turning 18.

Case study: Blu, Staying Well
Daniel, Blu’s Staying Well support worker, visits him regularly. This supports Blu to be more independent at home, where he feels more relaxed, and with less intensive psychiatric support. They support with benefits and administrative tasks that Blu finds difficult due to the challenges he experiences understanding letters.
Daniel also secured funding to contribute towards a new TV to provide Blu with a source of entertainment and manage his mood during his extensive periods spent indoors.
“I don’t like to go out very much. In my spare time I like to watch films, all types depending on the mood. Sometimes I read but I prefer films. It helps me to relax. Any time I feel down, I watch comedy which helps me feel better.
Blu spends most of his time in his flat. His social anxiety, mobility issues, joint pain, memory problems and paranoid schizophrenia mean that he finds leaving his home extremely challenging. He also needs frequent trips to the toilet, which tends to limit how far he wants to go or how long he stays out. The Staying Well team offers support that is sensitive to Blu’s needs and his desire to maintain a home of his own, while also helping him to manage his mood and the challenges he faces in interacting with the world outside his flat.’
My support worker, Daniel, has helped me feel more confident. He helps me to find the best solutions and to get better, and I’m very grateful for this. He gets me out of the house more. Most of the time we meet at the local bakery now, which is a big improvement.
If I didn’t get the support from Staying Well, I’d be half of what I am now, and I’d definitely be more depressed. They help me with anything to do with my health and getting the benefits I’m entitled to which means I can stay independent in my own home. To me this means a lot. What does home mean to me? Home is where the heart is.”
Can you help us?
We have a short survey that anyone who use our services will be invited to complete (online or on paper). It will take less than three minutes and will tell us how well we are doing and what we need to improve.